Continuous Glucose Monitoring (CGM) is used to gauge glucose levels in real-time throughout the day and night. A small electrode, known as a glucose sensor, is inserted under the skin to measure glucose levels in the tissue fluid. It is connected to a transmitter that sends the information via wireless radio to a monitoring and display device.
The primary use of CGM is for managing diabetes. It provides valuable insights into how exercise, food, and medication affect glucose levels, helping individuals with diabetes make proactive health decisions. CGM is a tool for more precise and personalized diabetes management, preventing unexpected highs and lows in blood glucose levels.
While CGM’s groundbreaking potential is widely recognized in diabetes management, it has recently been gaining attention in a broader context – for non-diabetic individuals. The concept of Continuous Glucose Monitoring for non-diabetics is rooted in the idea of proactive health management and optimization. It provides real-time insights into how different factors such as diet, exercise, and stress affect blood glucose levels, even without diabetes. This enables individuals to understand their body’s unique responses better, facilitating more informed lifestyle choices for optimal health and well-being. Despite this, the application of CGM in non-diabetics remains a relatively new field, with potential benefits and limitations that are still being explored.
This article explores the applications, limitations, and benefits of Continuous Glucose Monitoring for non-diabetics. It provides an overview of CGM’s potential uses for the non-diabetic population and delves into the key advantages and challenges of adopting this technology.
The Technology behind CGM

Continuous Glucose Monitoring (CGM) systems primarily consist of three essential components – a tiny sensor, a transmitter, and a receiver or display device.
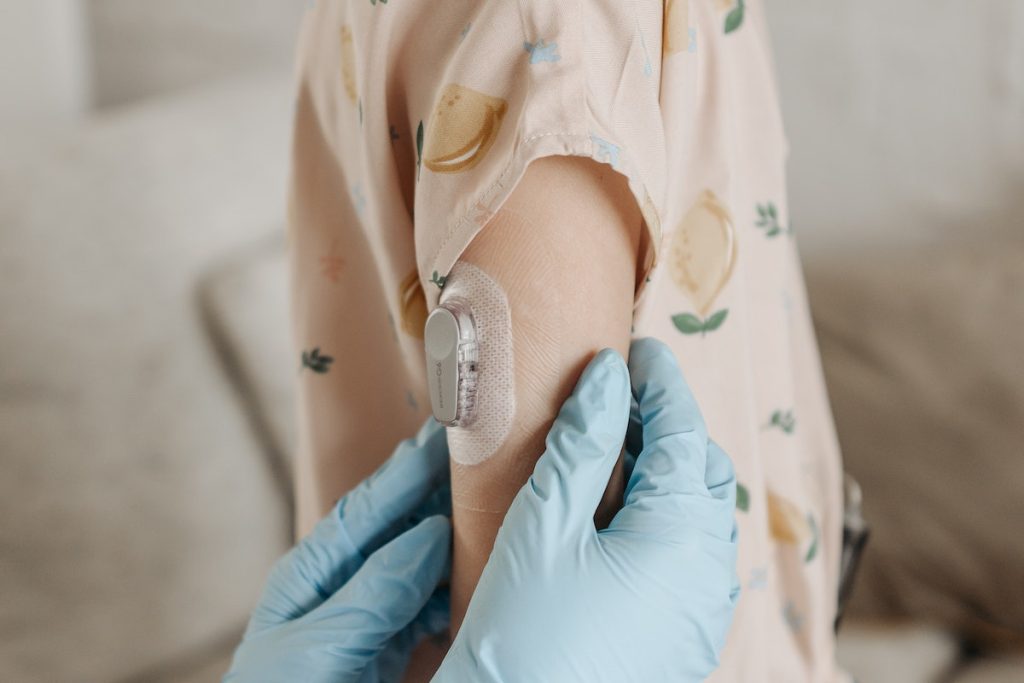
The sensor is a small, flexible filament inserted under the skin, often in the belly or upper arm. This sensor measures glucose levels in the interstitial fluid, which is the fluid around the body’s cells. Depending on the specific model, it is typically replaced every 7-14 days.
The transmitter is a small device that attaches to the sensor. It collects the glucose data from the sensor and wirelessly sends it to the receiver.
The receiver, a standalone device, a smartphone, or a smartwatch, receives and displays the glucose information. It provides real-time glucose readings every few minutes, trends showing whether glucose rises or falls, and alerts for when glucose levels are too high (hyperglycemia) or too low (hypoglycemia).
CGM technology provides a comprehensive view of blood glucose patterns and trends by providing these continuous readings. The dynamic data provided by CGM can be analyzed to make informed decisions about food intake, physical activity, and stress management – all of which can influence glucose levels.
Growth of CGM Adoption: A Statistical Overview
The adoption of Continuous Glucose Monitoring (CGM) has seen a significant surge in recent years, both within and beyond diabetes management. The global market for continuous glucose monitoring devices was valued at $7.816 billion in 2022 and is projected to grow at a compound annual growth rate (CAGR) of 4.4 percent from 2023 to 2030.
The increasing prevalence of diabetes and the rising adoption of continuous glucose monitoring (CGM) devices have been key drivers of this market growth. CGM devices offer a minimally invasive and effective solution for managing diabetes, enabling the detection of significant changes in blood glucose levels and preventing hypoglycemic conditions. These devices utilize sensors to analyze blood glucose levels at different intervals, with the readings transmitted wirelessly to diabetes management software. This technology empowers patients to understand their condition better and effectively manage it.
According to the International Diabetes Federation, the number of people diagnosed with diabetes in 2021 was approximately 536.6 million. This figure is projected to rise to 642.8 million by 2030 and 783.7 million by 2045. The CGM market’s estimated value is expected to reach $8.3229 billion by 2023, with a revenue forecast of $11.2 billion by 2030.
Interestingly, the increasing adoption of CGM isn’t confined to diabetes care alone. The trend of CGM usage among non-diabetics is also gaining momentum, driven by a growing awareness of proactive health management and the desire for personalized, data-driven insights into one’s health. It is, however, crucial to note that while the use of CGM among non-diabetics is growing, it remains a relatively new concept, and large-scale scientific data on its benefits and limitations in this population is still being accumulated.
Healthcare providers are showing an increased interest in the potential of CGM for non-diabetics, recognizing its value in providing a more thorough understanding of how various lifestyle factors affect individual glucose levels. This trend suggests that the usage of CGM in the broader population has the potential to rise in the coming years, contributing to the overall growth of the CGM market.
While these figures underscore the rapid advancement and acceptance of CGM technology, they also highlight the need for continued research and education to ensure its safe and effective use among non-diabetic individuals.
CGM Applications in Non-Diabetic Populations
Even without a diagnosis of diabetes, blood glucose levels continue to play a significant role in everyday health and wellness. Continuous Glucose Monitoring (CGM) provides a way for non-diabetic individuals to understand their body’s glucose patterns better, offering unprecedented insights into their metabolic health. CGM can help individuals monitor how their bodies respond to different foods, physical activities, stress levels, and sleeping patterns.
For example, an individual might discover that certain foods cause unexpected glucose spikes or that physical activity significantly impacts glucose dynamics. They might also identify how sleep quality or stress can influence glucose levels.
Understanding these patterns can help individuals make targeted dietary and lifestyle changes to avoid unfavorable glucose fluctuations. This level of data-driven personalization is key in optimizing one’s health, potentially preventing future metabolic disease, and enhancing overall well-being.
It is crucial to consult healthcare professionals before embarking on health optimization using CGM, as the data can be complex and requires professional interpretation. It’s also essential to remember that while CGM offers valuable insights, it still needs to replace the importance of regular medical check-ups and a balanced lifestyle.
CGM Use in Fitness and Sports Tracking
Continuous Glucose Monitoring (CGM) has been gaining momentum in fitness and sports, with athletes and fitness enthusiasts leveraging it to enhance their performance and recovery. CGM provides real-time feedback about how different types of exercise affect glucose levels, enabling a more personalized and effective training regimen.
For example, endurance athletes, like marathon runners or cyclists, might utilize CGM to ensure their glucose levels are adequately maintained during long training sessions or events. This data can guide fueling strategies, helping to prevent dips in performance due to low glucose levels.
Strength athletes or bodybuilders might use CGM to fine-tune their nutrition, particularly around workout times, to maximize muscle growth and recovery. The CGM data can help them determine the optimal timing and composition of pre and post-workout meals to ensure sufficient glucose availability for muscle protein synthesis while minimizing unnecessary blood sugar spikes.
In team sports, where energy demands can fructify drastically throughout a game, players might use CGM to understand how their glucose levels respond to different game situations. This can help devise personalized nutrition and hydration strategies to maintain optimal performance throughout the game.
Additionally, CGM can help track how the body recovers after strenuous exercise sessions. A spike in blood glucose levels following a workout can indicate that the body is recovering well, whereas persistently elevated glucose levels might signal ongoing inflammation and inadequate recovery.
However, it’s important to remember that while CGM can offer valuable insights into fitness and sports performance, the data should be interpreted with other performance metrics and under professional guidance to ensure a balanced and holistic approach toward health and fitness.
The Potential Benefits of CGM for Non-Diabetics
Continuous Glucose Monitoring (CGM) can offer non-diabetics a wealth of health insights beyond mere blood glucose levels. By providing a detailed, real-time view of glucose fluctuations, CGM empowers individuals with actionable data that can guide lifestyle modifications for better health.
Identifying food impacts
CGM data can help individuals understand how different foods impact their glucose levels. For instance, a person might notice that their glucose levels spike significantly after consuming a certain type of food, such as refined carbohydrates, and decide to limit their intake. Conversely, they may find that their glucose levels remain stable when they consume foods rich in fiber and protein, thus influencing them to incorporate more of these foods into their diet.
Understanding the effects of stress and sleep
The data derived from CGM can also demonstrate the impact of stress and sleep on glucose levels. Chronic stress and inadequate sleep can often lead to elevated glucose levels. By monitoring these levels, individuals can better understand the role of stress and sleep in their overall health and take steps to manage these areas effectively.
Optimizing exercise routines
CGM data can help in tailoring exercise routines to individual metabolic responses. Some people might find that their glucose levels drop dramatically during or after intense exercise, while others might notice a spike. This information can help guide exercise strategies, such as the timing and type of exercise and post-workout nutrition, to maintain stable glucose levels.
Facilitating weight management

For those striving for weight loss or maintenance, CGM can offer detailed insights into how the body metabolizes different foods and how particular eating patterns impact glucose levels and, subsequently, weight. This information can be pivotal in creating personalized diet plans that cater to individual metabolic needs.
These are just a few examples of the potential health insights gained from CGM data. The real-time, individualized data provided by CGM opens avenues for a more proactive, personalized approach to health management, setting the stage for potentially powerful preventive health strategies. However, while CGM data can be instrumental in guiding health decisions, it should be interpreted in the context of overall health status and lifestyle factors, ideally under healthcare professionals’ guidance, to ensure safe and effective application.
Limitations and Challenges of CGM in Non-Diabetics
While the benefits of CGM for non-diabetics are evident, one must also consider the limitations and challenges, particularly regarding data accuracy and reliability. Firstly, it’s imperative to acknowledge that CGM systems are primarily designed and calibrated for people with diabetes, where blood glucose levels frequently fluctuate beyond the normal range. Consequently, the accuracy of CGM readings in the normal glucose range, typically experienced by non-diabetics, might be lower.
Secondly, CGM measures glucose in the interstitial fluid rather than directly from the blood, potentially leading to discrepancies between CGM readings and blood glucose levels. Moreover, there could be a delay in glucose detection in the interstitial fluid, especially during periods of rapid glucose change, such as after meals or during intense exercise.
Additionally, factors like sensor placement, hydration levels, and even temperature can impact the accuracy of CGM readings. Therefore, while CGM offers valuable insights into glucose trends and patterns, it is not a substitute for professional medical advice. It should be used as a complementary tool in non-diabetic health management. It’s also critical that non-diabetic CGM users access accurate information and guidance on interpreting and acting on their CGM data.
CGM in Personalized Nutrition and Diet Optimization
Continuous Glucose Monitoring (CGM) opens a new window into personalized nutrition by providing real-time feedback on how the body responds to different foods. It enables individuals to identify specific foods or combinations that cause significant glucose spikes or crashes, leading to a more nuanced understanding of their dietary needs.
For example, some individuals might discover that certain high-carbohydrate foods, such as white rice or pasta, cause rapid and high glucose spikes. In contrast, others might find their glucose levels react more dramatically to sugary foods like desserts or soft drinks. In some cases, the pairing of foods can also influence glucose response. Some individuals may find that combining protein or fat with carbohydrates can moderate glucose spikes, providing valuable insights for meal planning.
CGM can also help individuals understand the impact of meal timing on glucose levels. For instance, some people might experience higher glucose spikes when eating the same meal late at night than in the morning.
By providing these personalized insights, CGM can guide individuals toward dietary changes that support more stable glucose levels. This, in turn, can contribute to better metabolic health, improved energy levels, and potentially prevent the onset of metabolic diseases. However, it is essential to remember that dietary changes should always be made in consultation with a healthcare provider since the interpretation of CGM data can be complex and should consider overall health, lifestyle, and dietary habits.
Examples of CGM-Guided Dietary Adjustments for Non-Diabetics
Making dietary adjustments based on Continuous Glucose Monitoring (CGM) data can be a game-changer in personal health management for non-diabetics. Here are a few examples of how CGM data might guide dietary changes:
- Moderating carbohydrate intake: CGM data might reveal that certain high-carbohydrate foods, such as bread or pasta, lead to significant glucose spikes for some individuals. Such individuals might decide to limit their intake of these foods or opt for whole-grain alternatives that have a lesser impact on glucose levels.
- Balancing meals: Some individuals might find that pairing carbohydrates with proteins or fats helps stabilize their glucose response. For instance, adding a source of protein like eggs or chicken to a carbohydrate-heavy meal might result in a more gradual rise in glucose levels.
- Considering meal timing: CGM data can provide insights into how meal timing affects glucose levels. Some individuals might notice higher glucose spikes when they eat the same meal late at night compared to earlier in the day. This might prompt them to rearrange their eating schedule, placing more carbohydrate-rich meals earlier when their bodies can better handle glucose fluctuations.
- Identifying food sensitivities: Some people might have unexpected glucose responses to traditionally healthy foods. For instance, someone might discover high glucose spikes after consuming certain fruits. This could lead them to reduce the portion size of these fruits or substitute them with others, resulting in a more stable glucose response.
- Tailoring snack choices: CGM might also guide snack choices. Some individuals may find that certain snacks, like a handful of nuts or a piece of dark chocolate, have a negligible impact on their glucose levels, making them a favored choice for between-meal nibbling.
These examples illustrate how personalized dietary adjustments based on CGM data can improve glucose control and overall health. However, it’s critical to interpret and apply this data in the context of overall dietary habits, lifestyle factors, and individual health goals, ideally with guidance from healthcare professionals.
CGM in Sleep and Stress Management
Continuous Glucose Monitoring (CGM) can be a powerful tool for monitoring sleep patterns and stress levels, contributing to a more holistic understanding of individual health and well-being.
Monitoring Sleep Patterns
Sleep profoundly affects glucose metabolism, with poor sleep often leading to increased glucose levels and insulin resistance. CGM can help individuals track glucose variations throughout the night and correlate them with sleep quality. For instance, frequent night-time glucose spikes might indicate disturbed sleep patterns or sleep disorders like sleep apnea. Similarly, despite not eating overnight, consistently high glucose levels in the morning could point to the phenomenon of “dawn phenomenon” or “morning hyperglycemia,” which is often linked to inadequate sleep.
Stress Management

Just like sleep, stress can significantly impact glucose levels. Both acute and chronic stress can lead to elevated glucose levels as part of the body’s “fight or flight” response. CGM can help individuals understand how stress events affect their glucose levels. Witnessing the direct impact of stress on glucose fluctuations can be a powerful motivator for individuals to explore and adopt stress management techniques such as meditation, relaxation exercises, or counseling.
Through tracking and understanding the linkage between glucose levels, sleep patterns, and stress, CGM can offer a valuable perspective on the importance of these factors in overall health. Nonetheless, interpreting CGM data about sleep and stress should be done under healthcare professionals’ guidance to ensure accurate understanding and appropriate responses.
Emerging Trends and Innovations in CGM Technology
Continuous Glucose Monitoring (CGM) has seen remarkable advancements in recent years, particularly in sensor technology. Innovations have focused on improving accuracy, extending sensor lifespan, enhancing user convenience, and expanding functionality.
Firstly, newer CGM sensors have improved accuracy, showing fewer discrepancies between interstitial fluid glucose readings and actual blood glucose levels. This advancement has led to more reliable data for users and greater confidence in CGM-guided decision-making, particularly vital for non-diabetics operating within the normal glucose range.
Secondly, the lifespan of CGM sensors has been extended, with some of the recent models lasting up to 14 days compared to the earlier 7-day lifespan. This extension reduces the frequency of sensor replacements, making CGM usage more convenient and cost-effective.
In terms of user convenience, the latest sensors have been designed to be more discreet and comfortable, with some models even offering the option of implantable sensors, minimizing the discomfort associated with frequent skin punctures. Some systems also allow sensor readings to be obtained without calibration fingersticks.
Furthermore, CGM technology is expanding its functionality. In addition to glucose monitoring, newer CGM devices can also measure and record other vital signs and health markers, offering a more comprehensive view of metabolic health.
These advancements in CGM sensor technology pave the way for wider adoption among non-diabetics, providing them with an accessible, reliable, and convenient tool for proactive health management. However, as CGM technology continues to evolve, it remains crucial that users understand the appropriate use, potential limitations, and the importance of professional guidance in interpreting CGM data.
The Future of CGM for Non-Diabetics
While Continuous Glucose Monitoring (CGM) has been pivotal in glucose management, its potential applications extend beyond just monitoring blood sugar levels. The wealth of data collected from CGM can offer valuable insights into other aspects of metabolic health and overall wellness, making it a promising tool in preventive healthcare.
One such application could be in the field of gut health. Emerging research suggests a strong link between gut microbiota and glucose metabolism. The real-time glucose data from CGM can help understand an individual’s gut health, guiding dietary interventions to improve gut microbiota.
Additionally, CGM data could be instrumental in managing hormonal health. Hormonal imbalances can significantly affect glucose metabolism. Hence, identifying glucose patterns might provide insights into hormonal dysfunctions and aid in personalized hormonal therapy.
Furthermore, CGM can also play a substantial role in research and clinical trials. The real-time and personalized glucose data can help researchers identify individual and population trends, enabling them to develop more targeted and effective treatments for metabolic disorders.
As the CGM technology evolves, so will its potential applications. Its ability to provide real-time, individualized metabolic information could revolutionize preventive healthcare, enabling proactive health management in non-diabetics. However, such potential applications should be backed by rigorous research to ensure safety and efficacy.
Ethical Considerations and Data Privacy
Continuous Glucose Monitoring (CGM) systems raise critical ethical considerations, as with any technology that collects personal health data. First and foremost is the issue of privacy and data security. CGM devices generate a wealth of personal health data that, if not appropriately safeguarded, could potentially be exploited by unauthorized parties. CGM manufacturers must prioritize data encryption and secure data transmission to protect user privacy.
The issue of data ownership also emerges in the discussion. Arguably, the data generated by CGM devices belongs to the users themselves. These users should be able to control who has access to their data and how it is used, including for research purposes. Therefore, consent mechanisms should be in place, allowing users to opt in or out of data sharing and be informed about who has access to their information and for what purpose.
Furthermore, equity in access to CGM technology is another ethical concern. As it stands, CGM systems are costly, and their cost might exclude certain sections of the population from benefiting from this technology. As CGM becomes more prevalent, addressing this digital divide becomes crucial to ensuring everyone can benefit from this technology.
Lastly, healthcare providers’ role and ethical responsibility in interpreting and advising on CGM data should not be overlooked. With the wealth of data that CGM provides, there is a risk of it being misinterpreted or taken out of context by users. Healthcare providers are responsible for providing accurate interpretation and guidance based on this data to prevent potential harm to users.
Therefore, while CGM technology has immense potential in personal health management, it is essential to consider these ethical implications and establish robust safeguards to protect user privacy, ensure equitable access, and promote responsible use.
Conclusion
Continuous Glucose Monitoring (CGM) holds significant potential for non-diabetic individuals, offering real-time data to guide personalized dietary adjustments for better metabolic health. It also provides insights into sleep patterns and stress management, contributing to a more holistic understanding of health. The ongoing advancements in CGM technology, such as improved accuracy, extended sensor lifespan, and expanded functionality, promise to increase its adoption among non-diabetics. Potential future applications of CGM data could extend to areas like gut health management, hormonal therapy, and clinical research. However, the use of CGM technology has limitations. It raises critical ethical considerations regarding data privacy, ownership, and equitable access. There’s an inherent risk of misinterpretation of CGM data by users, underscoring the crucial role of healthcare professionals in accurate interpretation and guidance. As CGM usage grows among non-diabetics, it’s essential to ensure responsible use backed by rigorous research and robust data safeguards.